State health officials are stepping up support to long-term care facilities, which have suffered 113 of Minnesota's 160 COVID-19 deaths, but urged people not to be complacent about the broader risks.
The concentration of deaths in older and sicker long-term care residents reflects the lower circulation of the virus under the statewide stay-at-home order and the preservation of hospital services that are saving lives in lower-risk cases, said Jan Malcolm, state health commissioner.
"The potential for it to spread quickly and widely and have some very negative consequences in the broader population is still there," Malcolm said. "As much as we are rightly focusing on long-term care, this is still a broad, populationwide risk."
Fourteen of the 18 deaths reported Tuesday involved long-term care residents, mostly in Hennepin County.
In a conference call with long-term care leaders, state health officials discussed ways to protect residents beyond the visitor restrictions and personal protective gear requirements for staff that have been in place for weeks.
Amid irregular supplies of testing for the new coronavirus that causes COVID-19, the providers discussed the broad use of pulse oximeters to monitor oxygen levels — which plummet when infected people begin to suffer severe illness, said Kris Ehresmann, state infectious disease director.
"That could be a useful tool," she said. "It's not something that has been implemented on a widespread basis."
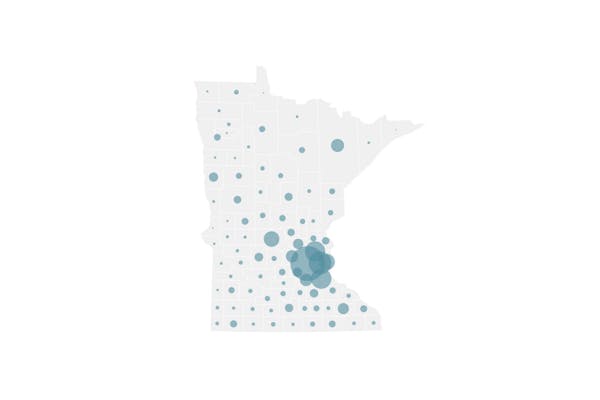
State health officials stressed the need for continued social distancing. Cases of lab-confirmed infections have been found in all but nine Minnesota counties, and totaled 2,567 on Tuesday.
The number of hospitalized cases remained at 237 for a second day, with the number of patients needing intensive care declining by nine.
M Health Fairview on Tuesday unveiled plans to add COVID-19 units in St. Joseph's Hospital in St. Paul and Southdale Hospital in Edina — a reflection of the demand hospitals are still anticipating. The system converted the Bethesda hospital in St. Paul into a 90-bed COVID-19 treatment center, but it is nearing capacity.
"While we recognize a COVID-19 surge may still be weeks away, we want to be fully prepared to respond to a rapid acceleration of cases," M Health Fairview officials said in a written statement.
At the start of the pandemic, state epidemiologists chased down anyone who had been in contact with an infected person who had already developed symptoms. Now, Ehresmann said they track down people who have been in contact with infected people 48 hours before their symptoms emerged.
Finding and then quarantining people potentially exposed to the virus benefits the community and long-term care facilities that can't entirely be walled off, Ehresmann said.
"There are a number of individuals who absolutely must be going into these facilities because they provide care, because they're providing meals, any number of services," she said. "That becomes the challenge. We cannot absolutely lock them down from interaction with the community."
The Star Tribune has received death certificate data from 105 confirmed COVID-19 deaths. Only 11 were younger than 70, and they tended to have underlying health conditions such as kidney disease, obesity, multiple sclerosis and heart disease that were listed as contributing to their deaths.
Deaths were split among male and female long-term care residents, but were more common among men (27) than women (10) who weren't living in such congregate care facilities.
Deaths included a nurse, 60; personal care attendant, 65; pharmacy assistant, 64; and therapist, 69. The records don't indicate if they were working or retired, though.
Health officials on Tuesday echoed comments by Gov. Tim Walz about the need to prepare for months of social distancing — even if the stay-at-home order is lifted on schedule on May 4.
The governor has called for a dramatic increase in testing for COVID-19, at a rate of 5,000 molecular diagnostic tests of nasal or throat swabs from suspect cases per day.
As of Tuesday morning, the state had reported 47,679 tests by public and private labs since March 29. The daily pace of testing has slowed over the past week, but labs have proposed rapid increases — including a $20 million proposal by the University of Minnesota to have capacity for 10,000 daily diagnostic tests and 10,000 antibody tests to see who has recovered from their infections.
Malcolm said the irregular testing — with health systems in some regions of the state having more supplies than others — has complicated efforts to protect long-term care facilities, because some haven't been able to immediately test workers and residents.
"It's been everybody on their own, so to speak, and what we're really trying to knit together now is a much more systematic approach … that can really make sure that everybody that needs to be tested will be tested," she said.
Despite testing shortages, health officials expressed confidence in national comparisons showing that Minnesota has had one of the lowest rates of COVID-19.
Cases are expected to rise in Minnesota at the end of the state-at-home order, which was designed to reduce face-to-face contact and disease transmission by 80% and give hospitals time to add more beds and equipment.
"We are feeling like we've made good use of the time," Malcolm said.
The state has already seen flare-ups, such as the widespread infections among workers in Worthington that caused the shutdown of the JBS pork plant. The case count in Worthington and surrounding Nobles County is 101. On Monday, state health officials reviewed 41 cases in that county and found that 33 involved JBS workers and six involved their relatives.
Jeremy Olson • 612-673-7744
Glenn Howatt • 612-673-7192

Want to share info with the Star Tribune? How to do it securely

'Safe recovery sites' would offer syringes, naloxone and more to people using drugs. The plan could be in peril.
New Minnesota GOP leaders seek peace with party's anti-establishment wing

Who is Republican Lisa Demuth, Minnesota's first House speaker of color?