Minnesota recorded its second death from COVID-19 and one of its largest single-day jumps in confirmed cases Thursday, underscoring the seriousness of the outbreak and the recent government "stay-at-home" order that takes effect at 11:59 p.m. Friday to combat the spread of the illness.
Both deaths involved Ramsey County residents in the 80s age range, though the cases are not related, the Minnesota Department of Health reported Thursday.
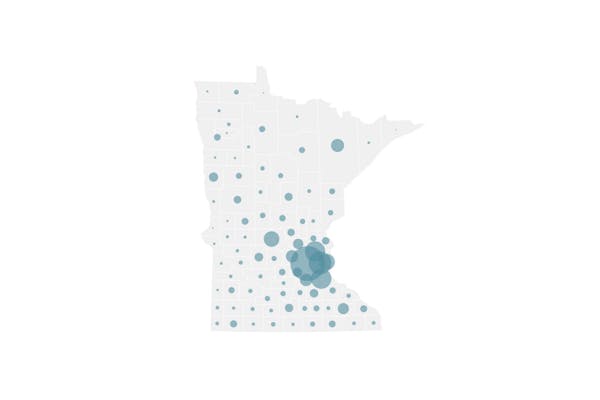
Testing has now confirmed 346 cases of COVID-19 in Minnesota since March 6, including 31 people currently hospitalized and 18 people receiving intensive care. The age range of cases is 5 months to 104 years.
Gov. Tim Walz said he worried that the shining sun and the small number of Minnesota deaths so far might make people complacent, but he urged them to follow the state orders and to consider the spike in cases and the 59 reported Thursday alone.
"Eight days ago," the governor said, "that would have been our total."
Of particular concern is the rise in intensive care usage. COVID-19 is caused by infection from a novel coronavirus, and while 80% of cases produce only mild symptoms, as many as 5% require intensive care.
The illness can cause severe breathing problems, requiring treatment with ventilators. But there are around 1,200 intensive care hospital beds in Minnesota, and only a fraction of them are open.
Modeling by the state health department and the University of Minnesota concluded that, in the absence of any mitigation efforts, the state would run out of intensive care beds in six weeks and see a peak in COVID-19 cases in nine weeks. Walz called that "unacceptable" due to the many people under that scenario who might die because ventilators would be unavailable.
Data analysis suggested that the state could push that peak in cases out to 14 weeks under a graduated series of social distancing restrictions.
Walz consequently issued his stay-at-home order for the next two weeks, and he plans to scale back to the current level of social distancing (including school and bar closures) for the three weeks after that.
If those steps prove successful in slowing the increase in cases, the next step would be to enforce the restrictions only for people in long-term care facilities or others at greatest risk of complications from COVID-19.
The state now has confirmed cases of COVID-19 in nine long-term care facilities and 18 residents of those facilities, said Kris Ehresmann, state infectious disease director.
Each has prompted a state response to reduce the risk of exposure to others, because global COVID-19 data have shown that the elderly and people with other health problems are at greatest risk of death.
"One case represents an outbreak if you will" in a facility, she said. "It can be a single case, and we take it very seriously."
State health officials provided more details Thursday about the data modeling that influenced the governor. The analysis was based on assumptions about how many ventilators are available, how often Minnesotans have face-to-face contact that presents an exposure risk, and how many people get infected by a single COVID-19 case.
It also was checked against the growth of cases in other countries that have deployed a variety of strategies to slow the pandemic.
However, state Health Commissioner Jan Malcolm declined to provide more specifics about the results of the modeling until they could be put in context for the public.
The modeling estimated 74,000 COVID-19 deaths in Minnesota had there been no mitigation efforts at all — a purely theoretical number because the state has already had schools closed for days and taken other social-distancing measures.
State officials have not disclosed how many deaths they expect under the current scenario of restrictions and executive orders that the governor has put in place.
"What we don't want is for people to get fixated on a specific number, as if that's a given," Malcolm said.
The current state goal is to delay the peak of cases and buy time for hospitals to add personal protective equipment to keep their workers healthy and on the job, and to add ventilators.
Walz earlier in the week said Minnesota is fortunate to have manufacturers locally, such as Ecolab and also Medtronic, which makes 15% of the global supply of ventilators. He said he has been reaching out to those companies to provide excess supplies to Minnesota.
While he acknowledged the ethical dilemma of lobbying for local products that are needed globally, the governor said he has little choice given the lack of a cohesive federal strategy for distribution and the encouragement by President Donald Trump for states to procure supplies on their own.
Hospitals have been pursuing a variety of solutions. Allina Health on Thursday recruited workers to volunteer in the assembly of face shields provided by a local manufacturer to protect caregivers.
M Health Fairview on Thursday completed its conversion of Bethesda Hospital in St. Paul into a 90-bed facility just for COVID-19 patients. Transfers of COVID-19 patients — including one who is critically ill — from other hospitals in that system started Thursday afternoon.
In only a matter of days, contractors equipped rooms throughout the hospital with negative-airflow systems, which reduce the threat of infected patients spreading the virus through coughing or sneezing.
The system transferred some doctors and nurses, and also added nurses from temporary staffing agencies to cover the need. At the current increase in hospitalizations and infections, the hospital could be full by mid-April, said Dr. Brian Amdahl, Fairview's vice president of medical affairs.
One goal in combining COVID-19 patients in one location is for the hospital to become a leader in the know-how of treating the illness, he said. "We can learn from every patient what's effective, what's not."
State emergency management leaders also continued to search for external sites to serve as overflow for hospitals, particularly for stable patients with conditions other than COVID-19.
While large arenas are being considered, state emergency management director Joe Kelly said closed nursing homes, dorms and hotels are more ideal.
"Those big, open spaces can create some significant challenges," he said, "in protecting already vulnerable patients from other infectious diseases like staph and norovirus."
Staff writer Glenn Howatt contributed to this story.
Jeremy Olson • 612-673-7744

Want to share info with the Star Tribune? How to do it securely

'Safe recovery sites' would offer syringes, naloxone and more to people using drugs. The plan could be in peril.
New Minnesota GOP leaders seek peace with party's anti-establishment wing

Who is Republican Lisa Demuth, Minnesota's first House speaker of color?