As the COVID-19 pandemic was ramping up aggressively in Minnesota in May, Cliff Willmeng was fired from his job as an Emergency Department nurse at United Hospital in St. Paul.
His offense? Wearing hospital-issued scrubs on duty while caring for COVID-19 patients, and then defying the hospital policy against nurses wearing uniforms that the hospital has to launder.
Willmeng is suing the 546-bed hospital to get his job back, saying his actions were compelled by personal safety, and the policy behind his May 8 firing was nonsensical. He joins a burgeoning group of hospital workers nationally filing lawsuits in response to what they see as pressure from hospitals to unreasonably lower safety standards for workers on the front lines of pandemic care.
"We have been seeing claims filed across the country by employees, or former employees, alleging they were terminated for raising concerns about PPE [personal protective equipment], or staffing, patient safety issues, all in connection with COVID-19. And I'm sure we are going to see more cases," said attorney Denise Dadika, co-chair of the health employment and labor group at law firm Epstein Becker Green.
United Hospital fired a second hospital nurse working with COVID-19 patients May 18, for failing to follow orders to watch an online training video at the hospital in April. That nurse, Monica Norberg, said the order conflicted with Gov. Tim Walz's mandate for remote work, because she could watch the video at home as she has done in the past.
Norberg has hired a lawyer, but unlike Willmeng, she's going through her union's grievance process before suing. When they were fired, both Norberg and Willmeng were union stewards with the Minnesota Nurses Association, whose members in United Hospital's Emergency Department organized a protest May 4 of the hospital's pandemic-safety practices.
A statement from Allina Health says the system follows the latest COVID-19 guidance from the Centers for Disease Control and Prevention and the Minnesota Department of Health. Hospital-issued scrubs are considered a uniform provided to employees working in sterile environments as a way to protect patients, unlike gowns worn over scrubs, which are considered PPE.
The health system declined to comment on employee situations, except to note in general that the health system prefers to resolve disputes through employee training.
"Our preference is always that education and coaching efforts will be successful," a statement from the health system says. "But we cannot appropriately retain employees who willfully and repeatedly choose to violate hospital policies designed to protect our patients and staff. Due to ongoing litigation, we won't be commenting further at this time."
After getting complaints about worker safety in the hospital, inspectors from the state Occupational Safety and Health Administration conducted an unannounced tour of the hospital May 5. That investigation remains open, according to federal documents.
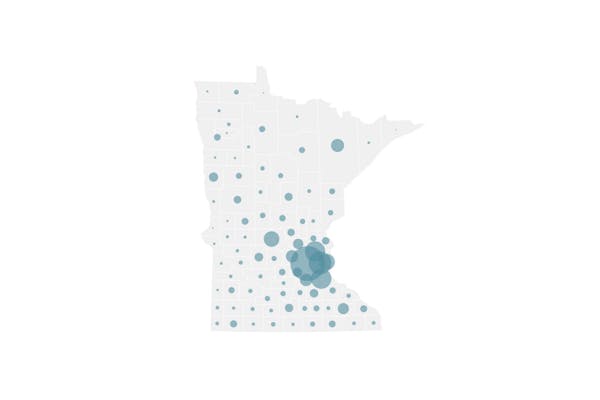
The safety of health care workers is not an abstract concern in Minnesota. So far, 6,805 health care workers in the state have tested positive for COVID-19 since March 5, including Norberg, who said she was put on paid "COVID leave" after she got the virus early in the pandemic.
Health care workers of all types comprise more than 10% of all known lab-confirmed cases in the state — a tally that stood at 60,898 as of Sunday.
The Minnesota Department of Health reported 806 new cases of the viral respiratory illness on Sunday and nine new deaths. Minnesota has seen at least 1,650 deaths from COVID-19.
Using seven-day averages to track broader trends, the average rate of COVID-19 fatalities peaked in Minnesota in late May and early June, but the rate of newly confirmed diagnoses is on par with the peak seen in late May, according to the Star Tribune's coronavirus tracking page.
Nationally, the United States has seen more than 5 million cases of the illness and about 162,000 deaths.
The scale of the unfolding COVID-19 pandemic, and the challenges posed by the gradually evolving scientific understanding of the SARS-CoV-2 virus, is what leads health care attorneys to expect more litigation from hospital employees.
Dadika, who represents employers in health care workplace lawsuits, said the increase in retaliation-related workplace claims at hospitals in recent months is understandable.
"Given the impact of the pandemic and the impact on individuals' health, especially as people watch the news and with what we've been seeing, it's not surprising," she said. "As much as we continue to learn about the coronavirus, there is still also so much we don't yet know, which is feeding into employees' concerns."
United Hospital has been criticized for providing hospital-issued scrubs to physicians but not nurses. The not-for-profit hospital's owner, Allina Health, has also been criticized for allowing nurses at sister hospital Abbott Northwestern in Minneapolis to wear the scrubs that nurses at United Hospital couldn't wear without a manager's approval.
The statement from Allina on Friday said Abbott Northwestern's practices on hospital-issued scrubs were changed over a month ago to be consistent with United Hospital's practice.
Willmeng said he didn't feel safe bringing his personal scrubs home after work, because the virus that causes COVID-19 can live on textiles for a period of time. United Hospital says scrubs are not a recognized form of PPE, and that the virus can be effectively removed from clothing with household laundry detergent at home.
The American College of Emergency Physicians published a guide this year that says high levels of exposure to the virus at work, combined with the possibility of asymptomatic transmission, puts health care workers at increased risk of transmitting the virus to family members and roommates.
"Hospital administrations and other organizations should assist HCWs [workers] in taking the necessary precautions to limit this risk, including providing fresh scrubs before each shift," the guide says.
But medical experts with Johns Hopkins Medicine say evidence suggests that the virus does not survive well on soft surfaces like textiles, compared with how long it can live on hard surfaces, like elevator buttons and door handles.
Willmeng questions why hospital administrators aren't more willing to collaborate with staff, given the shifting guidelines coming out of federal agencies and the considerable emotional toll on front-line caregivers. Besides, Willmeng says, there were plenty of professionally laundered scrubs to go around.
"Same-day surgery wasn't even happening, so all of the scrubs that would normally be used for surgeries were just sitting there," Willmeng said. "I knew that, Allina knows that. So it always felt like a power play."
Allina said the early days of the pandemic put great stress on its local and national suppliers, and even with the lower volumes of elective procedures it wasn't possible to increase the supply to issue scrubs to all staff.
"Allina Health has and continues to carefully weigh and adopt policies for the use and distribution of supplies," the statement said. "Our practices are aligned with other local and national hospitals and prioritize the safety of our staff and patients."

Want to share info with the Star Tribune? How to do it securely

'Safe recovery sites' would offer syringes, naloxone and more to people using drugs. The plan could be in peril.
New Minnesota GOP leaders seek peace with party's anti-establishment wing

Who is Republican Lisa Demuth, Minnesota's first House speaker of color?